Complex PTSD vs PTSD: What's The Real Difference
Not too long ago the words ‘trauma’ and ‘PTSD’ were words that one hardly ever heard, but we are living in a time with a plethora of information at our fingertips. ‘Trauma’ has become a massive buzz word, it isn’t just permeating social media but is becoming a part of everyday conversations. It is finally making its way into the mainstream and the general population is realizing it is way more common than just in war vets.
And yet, there are still many common misconceptions about trauma and the types of trauma categories there are. Many people don’t know the difference between Chronic PTSD vs Complex PTSD.
It’s important to be able to identify the correct type of trauma you have as it can provide insight into your symptoms and trauma responses. This clarity can help you to navigate your experiences in life, have clearer expectations about recovery and have better success on your healing journey.
What is Complex PTSD vs PTSD
The differences between Complex Post traumatic Stress Disorder vs PTSD are primarily related to the nature of the trauma experienced, the duration, and the resulting symptoms. Here is a breakdown:
PTSD (Post-Traumatic Stress Disorder):
Definition: PTSD is a mental health condition triggered by experiencing or witnessing a traumatic event, such as a natural disaster, serious accident, terrorist attack, war combat, or violent assault, etc.
Common symptoms include but are not limited to:
Intrusive symptoms - which involve involuntary, distressing recollections of the traumatic event. Examples of this include:
Reoccurring, involuntary and intrusive memories of the traumatic event.
Flashbacks, where the individual feels or acts as though the trauma is happening again
Disturbing dreams related to the trauma.
Intense psychological or physiological distress when exposed to conditions that resemble the event
Avoidance symptoms - which involve efforts to avoid reminders of the event. These behaviors include:
Avoiding memories, thoughts or feelings associated with the trauma
Avoiding external reminders such as people, places, conversations, or activities that arouse memories of the trauma
Negative alteration in mood and cognition, such as:
Persistent negative beliefs or expectations about oneself, others or the world. (e.g., “I am bad”, “The world is dangerous”)
Distorted thoughts about the cause or consequences of the trauma leading to self blame or the blaming of others
Persistent negative emotional states such as: fear, guilt, anger and shame
Diminished interest or participation in social activities or hobbies
Feelings of detachment or estrangement from others
Inability to experience positive emotions
Alterations in arousal and reactivity:
Irritable behavior and angry outbursts, with very little provocation
Reckless or self destructive behavior
Hypervigilance: being on alert or on guard
Exaggerated startle response
Difficulty concentrating
Sleep disturbances
Duration and Impact: Symptoms may occur shortly after the trauma and can last for months or years. PTSD becomes Chronic PTSD once the symptoms persist for more than a month.
Complex PTSD (C-PTSD):
Definition: C-PTSD arises from prolonged or repeated exposure to traumatic events, often in situations where the individual feels trapped, such as ongoing abuse, captivity, or chronic neglect. It is commonly associated with interpersonal trauma, like childhood abuse.
The symptoms of C-PTSD often overlap with those of PTSD, but may also include additional features:
Re-experiencing the trauma (similar to PTSD intrusive symptoms):
Flashbacks or intrusive memories
Nightmares related to the trauma
Intense emotional or physical reactions related to the trauma (e.g., seeing someone or something that triggers the trauma)
Avoidance and Numbing (similar to PTSD avoidance symptoms):
Avoiding reminders of the trauma, including people, places or activities
Emotional numbing, feeling detached or disconnected from others
Avoidance of emotions or shutting down feelings (e.g., anger, sadness)
Difficulty remembering aspects of the trauma
Affective dysregulation - which refers to difficulties regulating emotions and responses to distressing feelings:
Chronic feelings of emptiness or hopelessness
Intense feelings of shame, guilt or worthlessness
Mood swings, including irritability, anger or sadness
Difficulty controlling emotions, leading to outbursts or emotional instability
Feeling of being permanently damaged or broken
Interpersonal Difficulties - often involves problems in relationships and social functioning:
Difficulty trusting others, even in safe relationships
Persistent feelings of isolation, being disconnected from others or feeling a lack of belonging
Problems with self identity, such as feeling ‘like a different person’ or not knowing who you are
Difficulty with intimacy, often avoiding close relationships or having trouble forming healthy connections.
Negative Mood and Cognitions (can overlap with PTSD but is generally more pervasive with C-PTSD)
Negative self concept, believing oneself to be inherently flawed or unworthy
Pervasive feelings of hopelessness or despair about the future
Distorted beliefs about the trauma, such as blaming oneself entirely for the trauma
Inability to experience positive emotions or an emotional ‘numbness’
Duration and impact: Symptoms tend to develop over a longer period and can be more complex and deeply ingrained.
Similarities and differences between Complex PTSD symptoms and PTSD symptoms
As you can see Complex PTSD and PTSD are both trauma-related disorders, but they differ in their causes, symptoms, and duration. While PTSD can occur after a single traumatic event, C-PTSD develops as a response to ongoing trauma, leading to a broader range of emotional and relational difficulties.
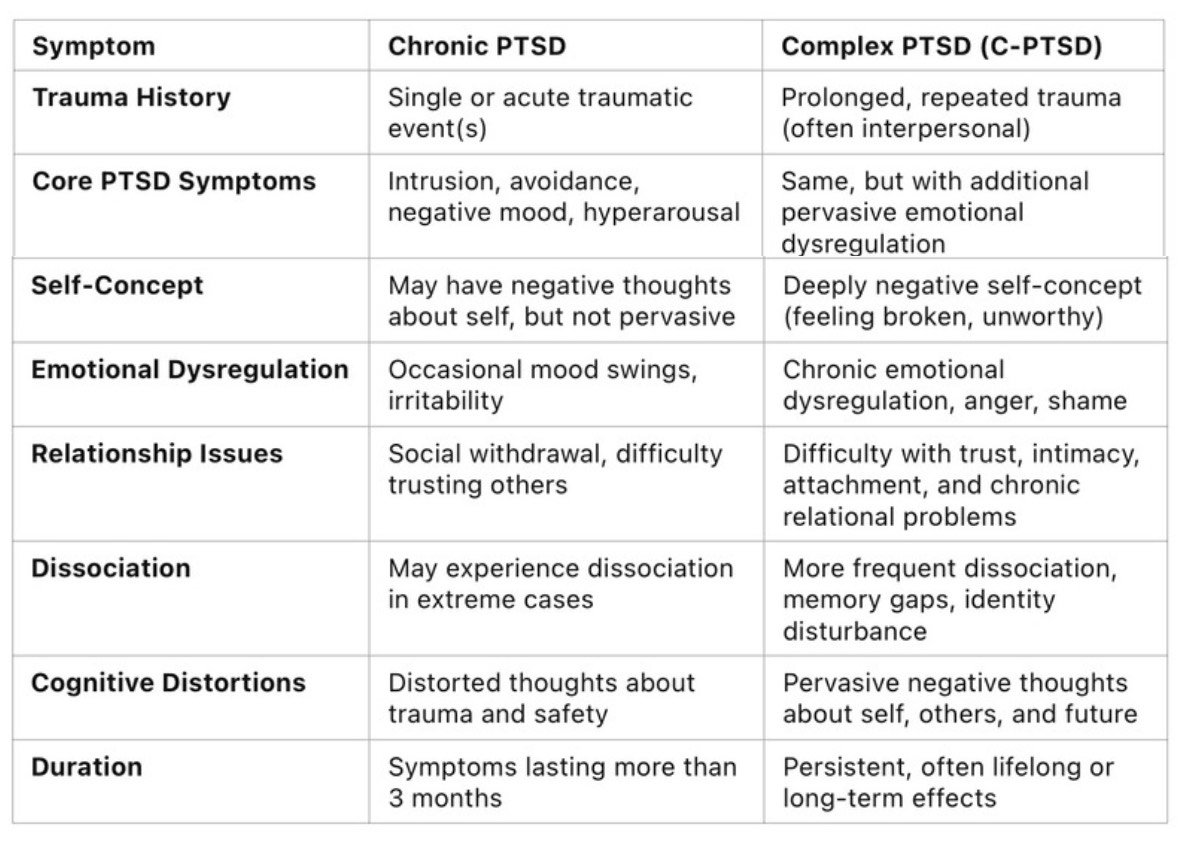
Here is a simplified graph to more easily compare the similarities and differences:
Now when it comes to Chronic PTSD vs Complex PTSD the differences remain the same. Chronic PTSD just means that the PTSD symptoms are lasting longer than one month, and as said above can last for months or years.
Understanding these distinctions can help you seek proper support and treatment. Because C-PTSD stems from prolonged trauma and is more deeply ingrained it generally requires a longer treatment period than PTSD. If you have identified with C-PTSD the information below can help you understand how the trauma you endured may be affecting your brain.
Unraveling the difference: The Complex PTSD brain vs the normal brain
The effects of C-PTSD on the brain can be profound, leading to noticeable differences when compared to a “normal” brain, which is defined as a brain that has not been subjected to chronic trauma or abuse. Research on the neurobiological impacts of C-PTSD shows how long-term exposure to trauma, especially in early childhood, can lead to structural and functional changes in the brain.
Here’s a comparison of the brain changes observed in individuals with C-PTSD versus those without trauma exposure:
1. Amygdala (Emotion Regulation and Fear Response)
In C-PTSD:
The amygdala is hyperactive in individuals with C-PTSD. This region of the brain is involved in processing fear and emotional responses. Chronic trauma can lead to an exaggerated fear response, heightened emotional reactivity, and increased anxiety.
In a “Normal” Brain:
The amygdala is more balanced and reacts to emotional stimuli in a measured way. In a healthy brain, it helps regulate emotional responses without overreacting to minor threats.
2. Prefrontal Cortex (Decision Making, Emotional Control, and Social Behavior)
In C-PTSD:
The prefrontal cortex (PFC), which is responsible for higher cognitive functions like decision-making, impulse control, and regulating emotional responses, can be underactive in individuals with C-PTSD. This results in difficulties with emotional regulation, impulse control, and decision-making. The PFC also helps dampen the overactive response of the amygdala, but in C-PTSD, this balancing function is often compromised.
In a “Normal” Brain:
The prefrontal cortex works efficiently to regulate the amygdala’s emotional responses, promoting better emotional regulation, decision-making, and planning. There’s a healthy balance between emotional responses and higher cognitive functions.
3. Hippocampus (Memory and Learning)
In C-PTSD:
The hippocampus, which plays a key role in memory formation and the processing of trauma-related memories, tends to be smaller or reduced in size in people with C-PTSD. This can lead to difficulties with memory, particularly in differentiating between past and present experiences (e.g., difficulty recognizing that a trauma is over, leading to hypervigilance or flashbacks).
In a “Normal” Brain:
The hippocampus is intact and works to process and store memories accurately, distinguishing between different memories and the context in which they occurred. This helps individuals keep past experiences in perspective and navigate new situations with appropriate emotional responses.
4. Anterior Cingulate Cortex (ACC) (Emotional Regulation, Pain Processing, and Cognitive Control)
In C-PTSD:
The anterior cingulate cortex (ACC), involved in regulating emotional responses and cognitive control, is often dysregulated in C-PTSD. This can contribute to difficulties in self-regulation, as well as an increased sensitivity to emotional pain and difficulty controlling automatic emotional reactions.
In a “Normal” Brain:
The ACC helps to regulate emotional states and is involved in modulating the emotional intensity of experiences. A well-functioning ACC helps with focus, reduces emotional overreaction, and facilitates problem-solving and coping.
5. Insula (Self-Awareness and Emotional Awareness)
In C-PTSD:
The insula, which is involved in awareness of bodily sensations and emotions, may become hyperactive in those with C-PTSD. This leads to increased emotional sensitivity and can contribute to heightened emotional distress. The insula also plays a role in the body’s stress response, which can be dysregulated in trauma survivors.
In a “Normal” Brain:
The insula functions to integrate sensory information and emotional responses, promoting a balanced experience of emotions and the ability to respond appropriately to them.
6. Default Mode Network (DMN) (Self-Reflection and Mind-Wandering)
In C-PTSD:
The Default Mode Network (DMN), which is active when the brain is at rest and involved in self-reflection, can become overactive in individuals with C-PTSD. This can contribute to rumination, intrusive thoughts, and re-experiencing traumatic events. People with C-PTSD may become stuck in negative thought patterns about themselves or their trauma.
In a “Normal” Brain:
The DMN is typically active in a balanced way, supporting healthy self-reflection, creativity, and mind-wandering without becoming stuck on negative or traumatic thoughts.
7. Neurotransmitters and Hormonal Systems
In C-PTSD:
Chronic trauma alters the neurochemical and hormonal systems involved in stress and emotional regulation. Key changes include:
Elevated cortisol levels (related to chronic stress) and dysregulated HPA (hypothalamic-pituitary-adrenal) axis function, leading to increased stress responses.
Imbalanced serotonin and dopamine systems, contributing to mood disorders like depression and anxiety.
Dysfunctional norepinephrine (noradrenaline) signaling, which is linked to hyperarousal, irritability, and difficulty sleeping.
In a “Normal” Brain:
Neurotransmitter systems are more balanced, with appropriate levels of serotonin, dopamine, and norepinephrine promoting stable mood, healthy stress responses, and good sleep quality. The body’s stress system (HPA axis) is activated in response to actual threats and returns to baseline once the threat is gone.
8. Structural Brain Changes
In C-PTSD:
Chronic trauma has been associated with shrinkage or atrophy in key brain regions such as the hippocampus, prefrontal cortex, and anterior cingulate cortex, as well as increased connectivity between the amygdala and other areas of the brain involved in stress responses. These structural changes can impair emotional regulation, memory, and overall brain functioning.
In a “Normal” Brain:
The brain’s structure is more resilient, with intact and functional communication between regions that help regulate emotions, thoughts, and memories. There is a greater ability to adapt to new experiences without long-term damage from short-term stress.
Conclusion
Understanding the differences between PTSD and Complex PTSD is crucial for both individuals experiencing trauma and the professionals supporting them. While PTSD typically arises from a single, often life-threatening event, Complex PTSD develops as a result of prolonged, repeated trauma, often occurring in abusive or highly stressful environments. Recognizing these distinctions not only helps in understanding the unique symptoms and experiences of those affected but also guides more effective treatment approaches tailored to the nature and duration of the trauma. Understanding the neurobiological effects of trauma, including how it impacts brain function, can also empower those suffering from PTSD or C-PTSD to engage in treatments that address both the emotional and physiological aspects of their trauma, promoting healing from the inside out.
As our awareness of trauma expands, it’s important to break down the stigma and misconceptions that often surround these conditions. Trauma, whether simple or complex, is not something to be ashamed of, and healing is possible with the right conditions and support.
Through my own journey of healing and transforming my trauma, and through helping my clients I have come to see how unique each persons trauma patterns can be as well as each persons journey through the threshold of trauma healing. If you are interested in somatic experiencing check out this page to learn more or you can always contact me directly.
I’m here to help you heal so you can begin to live the life of your dreams
My private practice specializes in helping people who have endured trauma, resolve the symptoms out of their body, mind & spirit so they can feel comfortable in their skin, find inner peace and live the desires of their heart.
I am based out of South Orange County, Ca and offer online therapy sessions. Whether you are just starting your healing journey or ready to try something new, I am here to help.
Do you have body trauma?
Did something ‘happen’ to you and your body and since then you are different, and can’t quite find your way back to yourself?
Are you longing to feel at ease and comfortable in your own skin?
Are you feeling stuck and blocked in uncomfortable painful patterns?
Get my FREE guide “Get Unstuck! The Truth About Body Trauma and How to Break Free’ and learn how to release trauma and create the future of your dreams. Plus, I will send you a few extra resources!